Faculty Focus with Dr Liam McKnight: Tips and Tricks to Pass
Revise Radiology
August 4th, 2022
An Interview with Dr Liam McKnight
This is an edited transcript of a talk given by Dr Liam McKnight for a Revise Radiology FRCR 2B Course. Before we dive into the article, here is a short introduction of Dr Liam McKnight.
Dr McKnight has worked as a general Radiologist with broad interests, including urogynecology. He was an FRCR Examiner for 6 years and was Chief Examiner for a further 5 years. He was an Examiner for the European Diploma in Radiology for 6 years and chaired the oral committee. Dr McKnight is an Examiner for the Anatomy exam for the Fellowship in Radiology of the Royal College of Surgeons in Ireland.
Dr McKnight has examined overseas in Hong Kong and Kuala Lumpur. Also in Singapore and Sri Lanka as well as some European countries.
Here's what you can learn from this article:
An Overview of The FRCR: A Threshold Examination
The Marking Scheme for the Vivas
Passing the Longs
The Marking Scheme for the Rapids
The Exam From the Examiners’ Perspective
Most candidates tend to undermine themselves by nervousness and stress. If you can take the exam like a normal out-patient session, you might be able to do better.
An Overview of The FRCR: A Threshold Examination
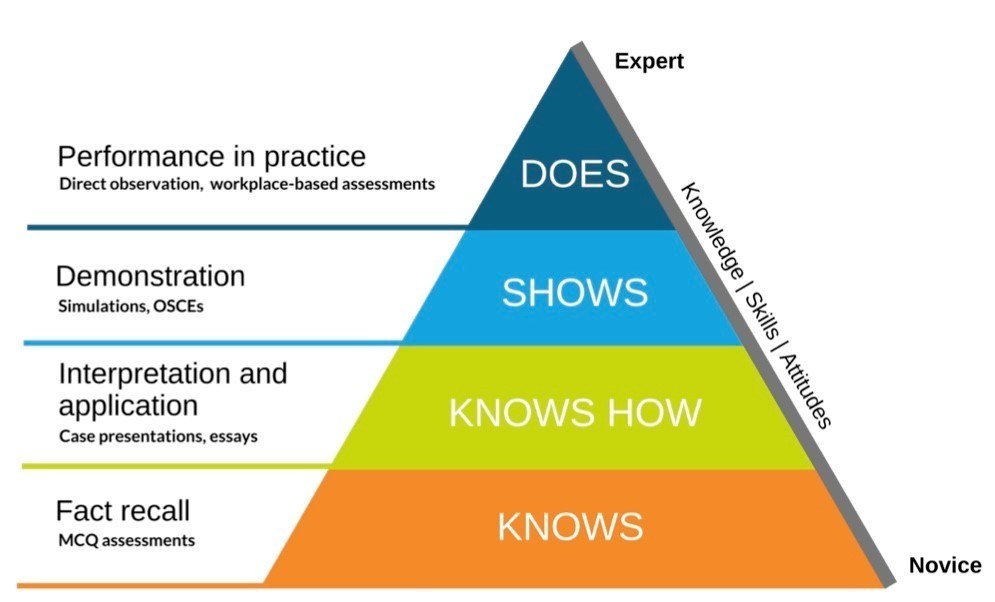
Miller’s pyramid to assess clinical competence has changed the way of examining in the last twenty years. Medical exams test:
Knowledge (how much you know) - whether you can memorise stuff,
Competence (whether you know how to do it)
Performance (can you show how)
Action (can you do it).
The apex of the exams is work-based assessments. Whether you are performing these with competence and with some fundamental knowledge.
FRCR is also a threshold exam – a binary choice, you are either over the line or you are not. To summarise the exam: “Are you safe?”
If you are not safe, the examiners will ask you to go back, revise more, prepare more and return. So, you need to practice, practice and practice, with guidance and feedback. You do this on a daily basis, till you are able to make it.
What do you really need to learn?
In FRCR 2B, we give you a broad range of materials, with a mixture of modalities and cases. This helps to assess whether you are ready to complete your core training.
The exam comes after the mid-point of a five-year training programme. So you should complete it in a little over three years. What we are trying to see is whether you can practice radiology in a competent way.
Part 2B is predominantly a skills-based exam.
FRCR 2B marking scheme:
Two oral structured exams, each marked separately
Two written exams RR and Reporting, each marked blindly from 4-8
24 is a pass
Borderline candidates are reviewed separately
The examiners will usually ask open questions which may not be easy to answer. If a candidate is indecisive, the examiners may question them further to get them off the fence. They will repeat the clinical information, if necessary. If the answers are vague, they will ask for a final answer.
Examiners will not necessarily give feedback so your final answer will be noted. Candidates may find this difficult as in a tutorial you are told if you have given the correct answer.
The Marking Scheme for the Vivas
The viva cases vary quite a lot. Some of the cases may be quite difficult, and some quite straightforward. What the candidates find difficult or easy depends on what kind of cases they are used to seeing.
One of the changes I made as Chairman was, the Faculty had to write down their material and present it in advance. We could vet it, and make sure that the candidates got a broad range of cases. They covered a variety of pathology, modalities and body systems.
How do radiologists work? Keith Simpkins said that radiologists are SAD people. Meaning that we See, Abstract and Deduce. These are quite different skills.
At the beginning of your career, you should be able to see the abnormality (not much good if you can’t see it). You have to then figure out what is it, and take into consideration the age of the patient and a bit of clinical info. You can then come up with a structured report. There will usually be a differential diagnosis. Based on your observations, one is usually the most likely.
The marking scheme is criterion-referenced for each case. There are no absolute criteria for passing or failing and there are no single killer cases. We all make mistakes. Marks are awarded for each case in a range from 4 to 8. What follows is based on the examiner's guidance when I was chair of the Examination Board.
4 is a very poor answer
Key findings are missed even with help. E.g. Did you miss the pneumothorax and the mediastinal shift?
Did you miss the mastectomy even though you were asked to check?
Did you make a completely wrong diagnosis? E.g. An enchondroma which is a non-aggressive lesion identified as a sarcoma. That is wrong and dangerous.
Did you make dangerous management statements?
Does the candidate understand the urgency of the situation? When should you write a letter or a report? When should you pick up a phone and speak to someone immediately?
6 is a bare pass
You have seen most of the principal findings. We may have given you some help, and the principal diagnosis is correct.
Suppose you get a case of bilateral hilar lymphadenopathy. Mention three of the main causes, TB, sarcoidosis and lymphoma.
If it's something rare, You can still pass, even if your ultimate diagnosis isn’t quite correct. You may have a limited differential, instead of five, you may have only three.
To get 8, all your findings have to be correct.
You interpret the findings well. You give a succinct and accurate report. You don’t make your reports too long. There’s an excellent differential and no significant errors.
How do the Examiners mark cases?
The examiner marks each case separately. One examiner will be talking to the candidate and making a few notes. The other one makes copious notes. Where the candidate is borderline, they use detailed notes if they need detailed feedback.
It is good not to spend too long on any single case. It’s difficult for the Examiners to judge anyone based on a single observation. The Examiner should stop a case where the candidate struggles for too long. This can be difficult for the candidate who wants to finish the case
In general, the Examiner should get through at least 5 cases in 15 minutes.
There may be more plain films than cross-sectional imaging. Electronic cases also may take longer if there are IT delays.
There will be a mixture of cases, modalities and pathology. There may be at least one multi-modality case. This is to see if the candidate can synthesise a report based on CT and MR or a radiograph and a bone scan.
There are no killer questions, if you have bungled a case, move on. There is no minimum number of cases, The candidate should not rush, but rather be safe and measured. The last time I examined, I went through around 200 scripts. The maximum number of cases seen by a failed candidate was 14 in half an hour. The minimum number of cases seen by a passed student was 7.
Common problems in oral exams are:
Missed key observations
Poor interpretation of abnormalities
Failure to use clinical information
A scattergun (unsystematic) approach
Indecisive conclusions
Unsafe diagnoses.
It may be helpful for the examiner to have these on the sheet to structure any feedback. This is also very useful when practising with candidates before the exam
Passing the Long or written cases
The long cases will be a mixture. There are usually six long cases from one of most of the following. Chest, abdomen, gynaec, neuro, urology, breast, paediatrics, MSK, GI.
There will be a mixture of pathologies. There will be a tumour, something congenital, infection, and some multi-modalities. Most UK candidates don’t fail the long cases. The mean mark is higher in the long cases. Unless you are barking up the wrong tree, it’s difficult to get it completely wrong.
The Marking Scheme for the Reporting
There are generally 6 cases covering most body systems. You must answer all 6
There will be a variety of pathology.
If you get 2 cases and you think both are TB or both are tuberous sclerosis, it is unlikely you are right. They will show you a mixture of cases.
Cases are mainly cross-sectional with some radiographs.
There will be mixed modality cases.
It is important that you practice the timing. You have to report 6 cases within 75 minutes. You need to make up for technological difficulties in loading the cases. You must spend at least 10 minutes on each case. The first marks are easy, you can probably get 5 out of 8 marks with just 20 words each.
Don’t write long essays. It’s difficult to get 7.5 out of 8, but it’s easy to get 4-6. So don’t spend too much time on any one case and complete them all
The Marking Scheme for the Rapid Reporting
Rapid reporting is difficult since you don’t get any feedback. There are 30 cases, you type your answers, and there is a complicated marking scheme.
There is a 10% permitted error rate and you have to get 27/30 correct to pass.
The easiest cases are abnormal cases.
Be wary of overcalling.
Timing is an issue. If you can get some of the clinical fractures easily that gives you more time.
There will be a couple of cases with 2 abnormalities in the film.
There are some half marks, so if you see spondylolisthesis, you get half a mark for the slip and half a mark for the defect. Similarly, for a head fracture with joint effusion, you get half a mark with the radial head fracture. And another half a mark for the joint effusion. You need both half marks, so that makes the marking scheme simpler.
In general, the examiner gives the arithmetic mean of your scores. So if you get 2 4s, 2 6s and 2 8s your average score is a 6. The examiner might adjust the score at the end
They may revise your score down if you make some significant or dangerous errors. If you get the basics right but didn’t know some of the subtler discriminating stuff, they may be more generous. Each examiner marks separately, but they agree on a final mark.
From the Examiners’ Perspective
It’s important for Examiners to give the same information to all candidates.
I don’t tell the diagnosis of the candidates. I give them the clinical information, but not the full history. Once they have the history, it is easier to work it out. There's a difference between knowing your patient is a 44-year-old Asian with a cough or the patient has a cough.
Were they making errors in observation and interpretation? - e.g., aggressive vs. nonaggressive. Did they use logic and deduction?
The examiner can talk about clinical management in patients and safety. The examiners compare the evaluations of borderline candidates to make sure they are fair.
Radiology is rigorous. Most radiologists are safe if they are systematic. In most cases, you start with the heart, then the lungs, then the ribs and the soft tissue and then the review areas.
Don’t be afraid to talk it through. The examiner marks you on what you say, and not on what you think, so it is important to build your confidence. Don’t be reluctant to speak out because usually, your first instincts will be right. The examiner might ask you to look behind the heart and then you see the lump. You may not score as highly if you get help, but you can still pass the case.
There may be many abnormalities. A mastectomy may be easy to spot, but can you see the other abnormalities? Are the bones are also abnormal? Not just the pleural effusion. If you link together the sclerotic bones and the pleural effusion, it’s usually a malignancy. If you look at the pleural effusions and stop, then you are missing out on points. And you also don’t get your diagnosis right.
Neonatal chest x-rays are often quite discriminating. RDS (surfactant deficiency) may have many abnormalities. Candidates usually look at the tubes and lines and fail to see the abnormalities.
In an x-ray, there may be a UA catheter and UA, a nasogastric tube, and bilateral airspace shadowing. Then a pneumothorax may be basal rather than apical and a mediastinal shift may be subtle.
If the candidate forgets the clinical information, the examiner may repeat it before coming to a conclusion. Imagine two radiographs which are relatively similar. In an adult, it could be renal cell carcinoma metastasis but that would be less likely in a child. So, use the clinical information. If you get nothing then say, in an adult, this looks like a metastasis but in a child, it could be round pneumonia
Avoid coming to premature conclusions. You may get a non-aggressive lesion, but you may come to a rapid conclusion, and say it’s a sarcoma. It’s difficult for a candidate to retract an answer but if you make a mistake, it’s better to go back and come to a different conclusion. It is better to go slowly and systematically.
In the case of a radiograph with many abnormalities, you will get more points if you spot them all. Like surgical clips which point to an operation, the soft tissue abnormality and the bone destruction help to diagnose it as a metastasis.
In the case of urgency, what would you do next? You can suggest what you do at your institution, there is no need for a perfect answer. For instance, in the case of an acute subarachnoid haemorrhage, 90% of the cases will be due to an aneurysm. So, ask for an angiogram. Some institutions do CT angiograms or MRI angiograms.
Linking observations. In a neonatal radiograph, the observations include an opaque left hemithorax and a loss of cardiac silhouette. It also consists of an ETT that is too far obstructing the left main bronchus, causing a left lung collapse. The candidate can link all these things. If the nasogastric tube had been pushed away from the lung abnormality, it could be due to expanding pneumonia or a large pleural effusion. Try and link things together.
My advice to candidates is to make and complete observations systematically. Don’t come to a rapid conclusion. Interpret the observations and link them to the history of the patient. Do a differential diagnosis and then come to a firm conclusion if possible. You can ask for occasional information, but not for the complete history. Try to be logical. Listen to your descriptions. Some candidates get so wound up that they give a certain description and then come to a different conclusion. Don’t give random diagnoses.
About the selection of material for the exam for the Vivas. The examiners will have a chest radiograph and a bone case. Also a mixture of modalities, a case involving a mixture of modalities, maybe more. The cases usually graduate from easy to difficult, starting with something straightforward. In each set, there will be 8-10 cases. The examiner will select cases and then the second examiner will complement these. It is unlikely they will both show pulmonary TB or gastric cancer. If a candidate is doing well, examiners will select more difficult cases. This is to establish the abilities of the better candidate and score them higher. If a candidate is struggling then select the simpler cases to see if they have mastered the basics.